Conditions We Treat- Cranial
Click the condition below to see more details
Traumatic brain injury
Aneurysm (Berry aneurysm)
Aneurysm or cerebral aneurysm is a cerebrovascular disorder in which there is a weakness in the wall of a cerebral artery which leads to a localized dilation of the blood vessel. The most common location of a cerebral aneurysm is the network of arteries at the base of the brain, termed the Circle of Willis. Aneurysms may result from congenital defects (coarctation of the aorta), preexisting conditions such as connective tissue diseases (Marfan’s syndrome), polycystic kidney disease or spurious - without a definitive cause. Aneurysms may also occur on the arteries that feed an arteriovenous malformation of the brain. Only very rarely are aneurysms inherited or passed on through a family. Cerebral aneurysms occur more commonly in adults than in children but they may occur at any age. They are slightly more common in women than in men. Occasionally a patient may have more than one aneurysm at the time of diagnosis.
Small aneurysms generally produce no symptoms. Due to the prevalence of brain imaging which is undertaken for a great variety of reasons, some aneurysms are discovered "incidentally"- an extra finding on the imagining study that was not related to the reason the study was ordered in the first place. Occasionally aneurysms can enlarge and put pressure on nearby cranial nerves or the brain and produce focal neurological signs or symptoms. Most aneurysms, however come to medical attention because they rupture. When an aneurysm ruptures, the individual may experience symptoms such as a sudden and unusually severe headache, nausea, vomiting, vision impairment, neurological deficits, and loss of consciousness. Onset is usually sudden and without warning. Rupture of a cerebral aneurysm is dangerous and results in bleeding into the subarachnoid space (subarachnoid hemorrhage), the brain itself, or into the cerebral ventricles.
Diagnosis of the cause of a subarachnoid hemorrhage involves CAT scanning, possibly lumbar puncture and ultimately cerebral angiogram. This test allows the visualization of the contour of the cerebral vessels and identification of the aneurysm.
Treatment of a ruptured aneurysm involves interruption of the blood flow to the aneurysm in an effort to prevent re-bleeding of the aneurysm. Treatment is usually carried out fairly quickly, since an episode of re-rupture of the aneurysm carries a significant risk of death. The risk of re-bleeding is highest in the first few days after the initial bleed.
The blood flow to the brain substance must be preserved during the treatment of the aneurysm. This treatment may be undertaken by clipping of the aneurysm which involves placing a titanium clip across the base of the aneurysm, thus stopping all blood flow to the aneurysm, or endovascular treatment (coiling) of the aneurysm, which involves the placement of coiled material into the aneurysm via very small catheters. This treatment causes clotting and scarring of the aneurysm. The choice of the specific type of treatment depends on the location and characteristics of the aneurysm and the patients medical condition.
Astrocytomas
Astrocytomas are called primary brain tumors - those that arise from the tissue of the brain itself. Astrocytomas are intracranial tumors derived from a type of glial cell called an astrocyte. These astrocytic cells serve as supportive cells for the neurons of the brain. Tumors from astrocytes may arise in the cerebral hemispheres, the cerebellum, the optic nerve, and the spinal cord.
The most common presenting symptom of an astrocytoma is the onset of a focal or generalized seizure. Between 60 to 75% of patients will have recurrent seizures in the course of their illness. Headache and signs of increased intracranial pressure (headache, vomiting) usually present late in the disease course. A Computed Tomography (CT) or Magnetic Resonance Imaging (MRI) scan is necessary to adequately visualize the tumor (size, location, consistency). All astrocytomas are malignant, but surgical biopsy however is necessary to diagnose and grade the astrocytoma, since these tumors are graded on a scale which describes the degree of dedifferentiation, aggressiveness and malignancy. Resection of tumors will generally allow functional survival for many years, and is the mainstay of treatment for this type of tumor. Generally, the more complete the surgical resection, the better the prognosis.
After surgical resection, radiation therapy or chemotherapy may be necessary. Astrocytomas often recur even after treatment and are usually treated similarly as the initial tumor, with sometimes more aggressive chemotherapy or radiation therapy.
In children, the tumor is usually located in the cerebellum and will present with some combination of gait instability, ataxia, and signs of increased intracranial pressure (headache, vomiting). Children with astrocytoma usually have decreased memory, attention, and motor abilities, but unaffected intelligence, language, and academic skills. Surgery again is the primary treatment for this type of astrocytoma- termed a pilocytic astrocytoma- and may be curative by itself.
Arteriovenous Malformation
Arteriovenous malformation (AVM) is a congenital disorder affecting the connections between the veins and arteries of the brain. The genetic transmission patterns of AVM (if any) are unknown, and AVM is not generally thought to be an inherited disorder. Normally, the arteries of the cardiovascular system carry oxygen-rich blood at a relatively high pressure. The wall of an artery is therefore fairly thick and strong. Arteries subdivide into the smaller arterioles, and then form capillaries. These capillaries are the very small abundant tubules which allow the diffusion of oxygen, carbon dioxide and nutrients to the bodies tissues. The capillaries are subsequently attached to venues-very small and low pressure vessels which drain into veins. In the case of an AVM, the capillary bed does not form, and instead the arterioles attache directly to the venules without the intervening capillary beds. This leads to several problems, the most significant of which is the fact that the venules and veins- structures designed to handle blood at low pressure - are now directly exposed to the high pressures of arterial blood. The veins become very dilated and are prone to rupture. On arteriogram films AVM formation often resemble a tangle of spaghetti noodles. This collection, often called a nidus, can be extremely fragile and prone to bleeding. This bleeding can be small and repeated, but on occasion may be devastating. It can cause severe and often fatal strokes. If detected before a hemorrhage, treatment is directed towards the occlusion of the arterioles which feed the AVM. This may be accomplished by craniotomy and surgical removal of the AVM, endovascularly with occlusion of the AVM vessel by glue and embolic particles- or a combination of the two approaches. The exact treatment depends on the size, location and complexity of the AVM
SYMPTOMS
AVM's of the brain usually present with hemorrhage or seizures. The symptoms of the hemorrhage depend on the site and severity of the bleed. Symptoms may include headache, nausea, vomiting, focal neurological deficit and coma. The vessels feeding an AVM may also give rise to cerebral aneurysms as a consequence of the very high rates of blood flow in these arteries. Diagnosis is made with CT, MRI and angiography.
TREATMENTS
Treatment can be with surgery, stereotactic radiosurgery, endovascular embolization, observation, or a combination of these treatments. Our group has specialty experience with all the modalities of brain and spinal cord AVM treatment.
Acoustic Neuroma
Brain Tumor
A brain tumor is any tumor within the intracranial space created by abnormal and uncontrolled cell division, either involving the brain itself (neurons, glial cells (astrocytes, oligodendrocytes, ependymal cells), the cranial nerves (myelin-producing Schwann cells), the coverings of the brain (meninges), skull, pituitary and pineal gland, lymphatic tissue, or metastatic disease from cancers located in organs other than the brain (metastatic tumors). Primary brain tumors- those tumors that arise from the cells that make up the brain itself- are commonly located in the posterior cranial fossa (cerebellum) in children and in the cerebral hemispheres in adults, although they can affect any part of the brain.
SYMPTOMS
Although there is no specific clinical symptom or sign for brain tumors, slowly progressive focal neurologic deficits, headache and signs of elevated intracranial pressure, as well as the new onset of seizures in a patient with a negative history for epilepsy are possible early signs and symptoms.
DIAGNOSIS
Imaging techniques such as computed tomography (CT) and magnetic resonance imaging (MRI) play a central role in the diagnosis of brain tumors. Electroencephalography (EEG) may also be ordered in a patient who presents with seizures. The exact diagnosis of a brain tumor is determined by examination of brain tumor tissue taken at the time of surgical resection of the tumor or biopsy of the tumor.
This histologic examination is often needed for determining the appropriate treatment of the tumor and helps determine if radiation therapy and or chemotherapy will play a role in the post-surgical treatment of the tumor.
Brain Aneurysm (Berry aneurysm)
Brain Aneurysm or cerebral aneurysm is a cerebrovascular disorder in which there is a weakness in the wall of a cerebral artery which leads to a localized dilation of the blood vessel. The most common location of a cerebral aneurysm is the network of arteries at the base of the brain, termed the Circle of Willis. Aneurysms may result from congenital defects (coarctation of the aorta), preexisting conditions such as connective tissue diseases (Marfan’s syndrome), polycystic kidney disease or spurious - without a definitive cause. Aneurysms may also occur on the arteries that feed an arteriovenous malformation of the brain. Only very rarely are aneurysms inherited or passed on through a family. Cerebral aneurysms occur more commonly in adults than in children but they may occur at any age. They are slightly more common in women than in men. Occasionally a patient may have more than one aneurysm at the time of diagnosis.
Small aneurysms generally produce no symptoms. Due to the prevalence of brain imaging which is undertaken for a great variety of reasons, some aneurysms are discovered "incidentally"- an extra finding on the imagining study that was not related to the reason the study was ordered in the first place. Occasionally aneurysms can enlarge and put pressure on nearby cranial nerves or the brain and produce focal neurological signs or symptoms. Most aneurysms, however come to medical attention because they rupture. When an aneurysm ruptures, the individual may experience symptoms such as a sudden and unusually severe headache, nausea, vomiting, vision impairment, neurological deficits, and loss of consciousness. Onset is usually sudden and without warning. Rupture of a cerebral aneurysm is dangerous and results in bleeding into the subarachnoid space (subarachnoid hemorrhage), the brain itself, or into the cerebral ventricles.
Diagnosis of the cause of a subarachnoid hemorrhage involves CAT scanning, possibly lumbar puncture and ultimately cerebral angiogram. This test allows the visualization of the contour of the cerebral vessels and identification of the aneurysm. Treatment of a ruptured aneurysm involves interruption of the blood flow to the aneurysm in an effort to prevent re-bleeding of the aneurysm. Treatment is usually carried out fairly quickly, since an episode of re-rupture of the aneurysm carries a significant risk of death. The risk of re-bleeding is highest in the first few days after the initial bleed.
The blood flow to the brain substance must be preserved during the treatment of the aneurysm. This treatment may be undertaken by clipping of the aneurysm which involves placing a titanium clip across the base of the aneurysm, thus stopping all blood flow to the aneurysm, or endovascular treatment (coiling) of the aneurysm, which involves the placement of coiled material into the aneurysm via very small catheters. This treatment causes clotting and scarring of the aneurysm.
The choice of the specific type of treatment depends on the location and characteristics of the aneurysm and the patients medical condition.
Cerebrovascular disease
Cerebrovascular disease is a term that describes disease affecting the arterial supply of the brain. Arteries may become blocked by a variety of pathological processes, including fatty deposits (atherosclerosis) or by blood clots; either through the process of embolization (clot migrating from another location and becoming lodged in the cerebral blood vessel) or by thrombosis (clotting of the blood within the cerebral blood vessel). The results of cerebrovascular disease can include a transient ischemic attack (TIA), a reversible ischemic neurological deficit (RIND) or a stroke. The main difference between these conditions is the time the neurological deficit is present; in the case of a TIA the deficit is present for 24 hours or less, a RIND’s deficits are present for less that two weeks and a "stroke" has permanent neurological deficits. The type of neurological deficit associated with any of these cerebrovascular-related events, of course depends on the location of the brain affected.
Chiari Malformation
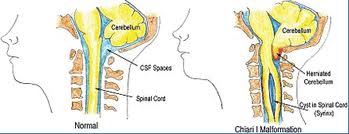
Chiari malformation is considered a congenital condition, although acquired forms of the condition have been diagnosed. This disorder is categorized in order of severity; types I, II, III, and IV. The term "Arnold-Chiari" is applied to the Chiari type II malformation. These malformations, are closely associated with syringomyelia and hydromyelia.
The cerebellum controls the coordination of motion, and is normally located inside the posterior skull, in what is referred to as the posterior fossa. Along the under surface of the cerebellar hemispheres, there are two small protrusions called the tonsils. These structures are located just above the foramen magnum, the largest opening at the base of the skull through which the spinal cord enters and connects to the brainstem.
Types of Malformations
Type I Chiari malformation
This malformation occurs during fetal development and is characterized by downward displacement by more than four millimeters, of the cerebellar tonsils beneath the foramen magnum into the cervical spinal canal. This displacement may block the normal pulsations of CSF between the spinal canal and the intracranial space. This form of Chiari malformation may be associated with
syringomyelia
Anomalies of the base of the skull and spine may also be seen in patients with Chiari I malformation. These possibly include bony abnormalities of the craniocervical junction (spina bifida occulta of arch of Ci, partial fusion of the vertebral arches of C1 and C2, Klippel Feil deformity and basilar impression of the spine resulting in brainstem compression.
Symptoms
Many people with Chiari I malformation have no symptoms. Many individuals complain of severe headaches, possibly associated with neck pain. The headache may be located primarily in the suboccipital area, and may be aggravated by coughing or sneezing. Many other patients complain of weakness of arms and /or legs, difficulty with balance, dizziness and blurred vision. Other symptoms related to a Chiari malformation are due to the development of a syrinx within the spinal cord. these symptoms include loss of pain and temperature sensation of the upper extremities, loss of strength and muscle mass of the hands and upper extremities, spasticity and difficulty with walking.
Type II Chiari malformation
This malformation is characterized by downward displacement of the medulla, fourth ventricle, and cerebellum into the cervical spinal canal, as well as elongation of the pons and fourth ventricle. This type occurs almost exclusively in patients with myelomeningocele.
Type III Chiari malformation
This malformation includes a form of dysraphism with a portion of the cerebellum and/or brainstem pushing out through a defect in the back of the head or neck. These malformations are very rare and are associated with a high early mortality rate, or severe neurological deficits in patients that survive.
Type IV Chiari malformation
This malformation is the most severe form and the rarest. The cerebellum fails to develop normally. There may be other associated malformations of the brain and brainstem. Most babies born with this malformation do not survive infancy.
Treatment
Treatment of Chiari malformations and syringomyelia is very dependent on the exact type of malformation, as well as progression in anatomy changes or symptoms.
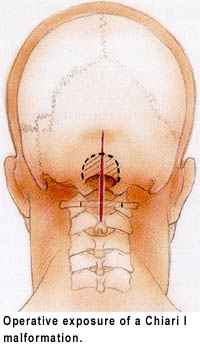
Chiari I malformations that are asymptomatic do not require surgery. If the malformation is symptomatic, or the cause of a syrinx, surgical treatment is usually recommended.
The goal of surgery is to relieve the symptoms associate with the Chiari malformation, and stop the progression of an associated syrinx if one is present. Chiari I malformations may be treated surgically with local decompression of the overlying bones and release of the dura (a thick membrane covering the brain and spinal cord). Rarely some degree of cerebellar tissue resection may be performed along with this decompression.
Decompression is performed under general anesthesia. It consists of removing the back of the foramen magnum and often the back of the first few vertebrae to the point where the cerebellar tonsils end. This provides more space for the brainstem, spinal cord, and descended cerebellar components. A tissue graft is often spliced into this opening to provide even more room for the unimpeded passage of CSF. This decompression of the craniocervical junction will allow resolution of the spinal syrinx symptoms in the majority of cases. Occasionally, the syrinx cavity within the spinal cord may be drained with a diverting shunt tube. Chiari II decompression is treated similarly, but is usually restricted to decompressing the tissues in the spinal canal and leaving the back of the skull alone.
Outcome
The benefits of surgery should always be weighed carefully against its risks. Although some patients experience a reduction in their symptoms, there is no guarantee that surgery will help every individual. Nerve damage that has already occurred usually cannot be reversed. Some surgical patients need repeat surgeries, while others may not achieve symptom relief.
Facial Pain (Trigeminal Neuralgia)
Trigeminal neuralgia is the most common of the neuralgia syndromes.
An estimated 1 in 15,000 people suffers from trigeminal neuralgia, although numbers may be significantly higher due to frequent misdiagnosis. It usually develops after the age of 40, although there have been cases with patients being as young as three years of age.
The pain associated with trigeminal neuralgia is intermittent and feels like bursts of sharp, stabbing, electric-shocks. This pain can last from a few seconds to a few minutes.
This intense pain involves the eyes, lips, nose, scalp, forehead, and/or jaw. Trigeminal neuralgia is considered by many to be among the most painful of conditions.
To describe the pain sensation, patients describe a trigger area on the face, so sensitive that touching or even air currents can trigger an episode of pain.
The intermittent sharp pain associated with trigeminal neuralgia interferes with common daily activities such as eating, speaking, laughing and sleep. They live in fear of unpredictable painful attacks, which leads to sleep deprivation and under eating. The condition can lead to irritability, severe anticipatory anxiety, depression and life-threatening malnutrition. Suicidal depression is not uncommon.
Some patients will have a characteristic muscle spasm which often heralds the onset of a painful attack. This muscle spasm led to the original term for trigeminal neuralgia termed "tic douloureux" ("tic", meaning 'spasm', and "douloureux", meaning 'painful', in French).
There are several different causes of trigeminal neuralgia and because people’s symptoms vary, many cases may go un-diagnosed or are difficult to diagnose. Some of the factors that contribute to trigeminal neuralgia are:
- Nerve damage or trauma relating to a dental procedure, surgery, or accident.
- A vessel that is pressing directly on the root of the nerve.
- A tumor pressing on the nerve. (rare)
- Advanced MS that can cause the Myelin Sheath that covers the nerve to deteriorate. (rare)
- Lyme Disease trigeminal neuralgia.
- Post-Herpetic (shingles) trigeminal neuralgia.
- Other viral infections.
Trigeminal Neuralgia Diagnosis MRI can be used to determine whether pathology such as a tumor or multiple sclerosis is irritating the trigeminal nerve. Otherwise, no test can determine with certainty the presence of trigeminal neuralgia. Tests can, however, help rule out other causes of facial disorders. Trigeminal neuralgia usually is diagnosed based on the patient's description of the symptoms.
Trigeminal Neuralgia Treatment
Medications may be used as a first line treatment for trigeminal neuralgia and are usually anti-seizure medicines. These include in particular "tegretol", "trileptal", neurontin" and "lyrica." If medication is not helping or patients are experiencing side effects from the medication, then a procedure can be considered.
The surgical treatment of trigeminal neuralgia includes several surgical procedures including microvascular decompression, radiofrequency rhizotomy, glycerol rhizotomy, balloon rhizotomy, and stereotactic radiosurgery).
Surgery may be recommended, either to relieve the pressure on the nerve or to selectively damage it in such a way as to disrupt pain signals from getting through to the brain. In trained hands, surgical success rates have been reported at better than 90 percent.
Of the five surgical options, the microvascular decompression (MVD) is the only one which preserves the trigeminal nerve and addresses the nerve compression by cerebral blood vessels when they are the cause of trigeminal neuralgia. In this procedure, the surgeon enters the skull through a small opening behind the ear. The nerve is then explored for an offending blood vessel, and when one is found, the vessel and nerve are separated or "decompressed" with a small pad. When successful, MVD procedures can give permanent pain relief with little to no facial numbness.
Nerve-Injuring techniques can also be very effective in treating trigeminal neuralgia. These methods of nerve injury include "percutaneous procedures performed through a needle, and radiosurgical procedures accomplished by use of computer-focused radiation beams.
Percutaneous trigeminal nerve injuring procedures, also known as "rhizotomies," use needles or catheters that enter through the face into the opening where the nerve first splits into its three divisions. Excellent success rates using these "percutaneous" surgical procedures have been reported.These techniques include "radiofrequency", glycerol" and "balloon" methods. In a radiofrequency rhizotomy, a surgeon uses an electrode to heat the selected division or divisions of the nerve. Done well, this procedure can target the exact regions of the errant pain triggers and disable them. This technique is particularly useful for patients with pain in the cheek or jaw, or the lower portions of the face. Glycerol rhizotomy involves injecting glycerol, an alcohol like substance, into the cavern that bathes the nerve. This liquid can injure the nerve just enough to disrupt the pain signals. Balloon compression involves compressing the nerve against the skull, again, just enough to stop the passage of pain signals. The balloon technique is particularly useful for patients with ophthalmic division pain, that is, pain in the forehead or eye.
Another procedure for treating trigeminal is stereotactic radiosurgery. In this technique, super-focused radiation beams are aimed at the nerve, to disrupt the pain signals. This procedure is a one day, minimally invasive, out-patient procedure, that does not require anesthesia. The procedure is done with only the most advances stereotactic radiosurgery devices such as the Gamma Knife, or specialized linear accelerators such as the Cyberknife. No incisions are involved in this procedure. Radiation is used to bombard the nerve root, targeting the same point where vessel compression is normally found. This procedure is particularly favorable for patients who are older, have serious medical problems, or who have to stay on blood thinners.
These nerve injuring procedures are useful for patients who are elderly, have significant medical problems, have failed MVD, or have multiple sclerosis (in whom blood vessel compression is not felt to be the cause of the trigeminal neuralgia). The nerve-injuring techniques are minimally invasive, out-patient procedures. The main disadvantages to these techniques include the risk of producing numbness or dysethesias (abnormal feelings) in the face as well as a higher chance of recurrence with time (because the nerve can regrow.)
Glioblastoma multiforme
Glioblastoma multiforme (GBM), also known as grade 4 astrocytoma, is the most common and aggressive type of primary brain tumor, accounting for 52% of all primary brain tumor cases and 20% of all intracranial tumors. Despite being the most prevalent form of primary brain tumor, GBMs occur in only 2-3 cases per 100,000 people in Europe and North America.
SYMPTOMS
The specific symptoms produced by this tumor is dependant on the area of brain involved the the pathological process. The single most prevalent symptom is a progressive memory, personality, or neurological deficit. These occur when the tumor affects the temporal, frontal lobesof the brain. Some other common symptoms of the disease include.
- seizure
- nausea
- vomiting
- headache
- weakness on one side of the body (hemiparesis).
The tumor can start producing symptoms quickly, but occasionally is an asymptomatic condition until it reaches an enormous size.
Most glioblastoma tumors appear to be sporadic, without any genetic predisposition. However, certain genetic disorders are associated with an increased incidence of gliomas, including Neurofibromatosis, Tuberous sclerosis, Von Hippel-Lindau disease, Li-Fraumeni syndrome, and Turcot syndrome.
No links have been found between glioblastoma and smoking, diet, cellular phones, or electromagnetic fields. Recently, some evidence for a viral cause has been discovered. Patients with a known "low-grade" astrocytoma (brain tumor), are at a higher risk of developing a GBM by the process of the lower grade tumor "jumping grades" by transformation of a part of the low grade tumor into a more aggressive form.
TREATMENTS
Glioblastoma is particularly difficult to treat for a variety of reasons. Its exact anatomical location within the brain may be the greatest limiting factor,since certain areas of the brain are more amendable to aggressive surgery (silent areas of the brain) and some are well identified as being home to critical brain function (the so-called eloquent areas of the brain). Depending on the site of the tumor growth, the treatment options may be broad or very limited. For the individual patient then, treatment may include all or a combination of chemotherapy, radiotherapy, and surgery.
Many drugs that are effective in other types of tumor are not able to cross the blood-brain barrier, and are therefore ineffective it the treatment of GBM. Compounding this difficulty is the fact that GBM tends to be particularly resistant to conventional tumor therapies. Nonetheless, many advances in microsurgical techniques, radiotherapy and chemotherapy are slowly increasing the survival rates of patients diagnosed with glioblastoma.
Surgery is the first and often the most effective treatment of glioblastoma. Surgery is useful in not only establishing the diagnosis through tissue biopsied for pathological analysi, but it has been shown that patient survival directly correlates with the degree of tumor removal- with complete gross total resection giving the best survival rates. It is sometimes feasible to remove only a part of the tumor, due to the tumors involvement with eloquent areas of the brain. In these cases, the surgical goals include biopsy to provide pathological diagnosis, "debulking" of the tumor to alleviate the symptoms of a large mass pressing against the brain, to decrease the number of residual cells to be addressed by radiotherapy and chemotherapy, and to prolong survival.
Generally, the greater the extent of tumor removal, the longer the survival time. Removal of 98% or more of the tumor has been associated with a significantly longer median survival time than if less than 98% of the tumor is removed.
Post-surgical radiotherapy is used to further treat the tumor. Three-dimensional conformal radiotherapy, which is targeted and more precise than whole-brain radiotherapy, is more effective at improving the patient’s survival. Radiotherapy is "fractionated"- that is the delivery of many small daily consecutive doese of radiation to the patient. In this circumstance the tumor is exposed to an almost constant bath of radiation, which has been shown to be more effective in treating these tumors since mores malignant cells are exposed to radiation as they go through the cell division process. This is important since it is during cell division that a cells DNA is most vulnerable to the ionizing effects of radiation which in turn can lead to the tumor cells death.
Chemotherapy is also used in conjunction with surgery and radiotherapy. Chemotherapy has been shown to increase patient survival, without much additional toxicity.
CNS Lymphoma
A central nervous system (CNS) lymphoma is a primary intracranial tumor appearing mostly in patients with severe immunosuppression (e.g. patients with AIDS, on anti-rejection drugs, etc.). CNS lymphomas represent around 20% of all cases of lymphomas in HIV infections.
In immunocompetent patients (that is, patients who do not have AIDS or some other immunodeficiency), there is rarely an association with EBV infection or other DNA viruses. In the immunocompetent population, CNS lymphomas typically appear in older patients in their 50's and 60's. Importantly, the incidence of CNS Lymphoma in the immunocompetent population has been reported to have increased more than 10-fold from 2.5 cases to 30 cases per 10 million population. The cause for the increase in incidence of this disease in the immunocompetent population is unknown.
Treatment includes surgical biopsy for pathological confirmation of the tumor, followed by chemotherapy. Radiation therapy may also be employed.
Gliomas
Gliomas A glioma is a tumor that affects most commonly the brain but occasionally the spinal cord. The tumor represents the malignant transformation of the supporting (non-thinking) cells of the brain and spinal cord called the glia. The exact causes of this malignant transformation are not known. Hereditary genetic disorders such as neurofibromatoses and tuberous sclerosis are known to predispose to the development of gliomas, and obesity during adolescence increased the risk by three to four times greater than having normal weight. Being tall also increased the risk; each 10 centimeter increase in height increased the risk nearly 20 percent.
TREATMENT
Treatment for brain gliomas depends on the location, the cell type and the grade of malignancy. Often, treatment consists of a combined approach, using surgery, radiation therapy, and chemotherapy. Surgery provides the options of biopsy of the tumor to establish diagnosis, debulking of the tumor to relieve the mass effect of the tumor on surrounding brain, and complete gross total resection of the tumor when the anatomical location of the tumor within the brain allows. The "adjuvant" or additional treatments of radiation therapy and chemotherapy are predicated on the results of the pathological evaluation of the surgical tissue, the extent of surgial resection, the size of the tumor cavity (or residual tumor) and the anatomical location of the tumor.
Hydrocephalus
Hydrocephalus is a term derived from the Greek words "hydro" meaning water, and "cephalus" meaning head. In years passed this condition was sometimes known as "water on the brain". People with this condition have abnormal accumulation of cerebrospinal fluid (CSF) in the one or more of the four cerebral "ventricles" - or cavities normally found within the brain. This may cause increased intracranial pressure with the resultant compression of the brain, headaches, decreased mental status, neurological deficits, seizures and in young infants progressive enlargement of the head and mental disability.
Hydrocephalus is usually due to blockage of CSF outflow in the ventricles or in the subarachnoid space over the brain. In a normal healthy person, CSF is formed in organs within the cerebral ventricles called the choroid plexus and continuously circulates through the ventricles towards it’s exit at the base of the brain just after the fourth ventricle through the foramen of Luska and Magendie. From those points the CSF circulates around the spinal cord and over the convexities of the brain where it is absorbed in structures termed the arachnoid granulations.
In the circumstance of hydrocephalus, the cerebrospinal fluid accumulates in the ventricles due to either a blockage of egress of the fluid from one or more of the ventricles, a failure of absorption at the level of the arachnoid granulations or rarely an overproduction of the fluid, Infants and young children with hydrocephalus typically have abnormally large heads, because the pressure of the fluid causes the individual skull bones which have not yet fused together to form a solid skull due to the patients young age to be pushed apart at the suture lines between these bony plates as a result of the expansion of the brain by the accumulation of cerebrospinal fluid within the ventricles. Compression of the brain by the accumulating fluid eventually may cause convulsions and mental retardation. Hydrocephalus occurs in about one out of every 500 live births and was routinely fatal until surgical techniques for shunting the excess fluid out of the central nervous system and into the blood or abdomen were developed.
In adults hydrocephalus may occur as the result of central nervous system infections (meningitis, etc.), as a result of head trauma, as a consequence of subarachnoid hemorrhage, tumor intraventricular hemorrhage or as a result of pre-existing conditions such as aqueductal stenosis.
Treatment for this condition most commonly involves shunting of the excess fluid from the cerebral ventricles to an area of the body which can absorb this excess fluid. Typically a ventriculo-peritoneal shunt is utilized- so named since the shunt originates in the ventricles, and terminates in the peritoneal cavity, which lines the abdominal cavity. Typically these shunts utilize a valve which can be set to restrict the amount of flow through the shunt. An alternative to a shunt is another operation called a third ventriculostomy. In this procedure, a small opening is made through the floor of the third cerebral ventricle, so that the accumulated cerebrospinal fluid can escape the ventricles and reach the arachnoid granulations. This surgery is utilized in the circumstance where the obstruction to the cerebrospinal fluid is within the ventricles and the function and access to the arachnoid granulation is normal.
Intracranial hemorrhage
An intracranial hemorrhage is defined as any hemorrhage ( bleeding ) within the skull. Intracranial bleeding occurs when an intracranial blood vessel ruptures or is torn/damaged. It can result from physical trauma (as occurs in head injury) or other non-trauma related causes such as a ruptured aneurysm. Intracranial hemorrhage is a serious medical emergency, and these patients require rapid medical evaluation and treatment. Patients often complain of severe headache, nausea, vomiting, weakness and dizziness. Focal neurological deficit may or may not be present due to the nature of the bleed and the area of the brain which may be involved.
Radiographic evaluation, which may include CAT scan (computed axial tomography), MRI and or cerebral angiography may be employed to make a definitive diagnosis. Subsequent treatment is predicated on the nature, size and location of the hemorrhage taken together with the clinical status of the patient.
Meningiomas
Meningiomas are the most common benign tumors of the brain (95% of benign tumors) and overall represent about 15% of all intracranial tumors. Rarely they can be malignant. Meningiomas can arise anywhere arachnoidal cap cells are located, and therefore are found within the spinal canal and even the cerebral ventricles. They arise from cells which help form the meningies called the arachnoidal cap cells. They are more common in females than in males (2:1) and in some cases have estrogen receptors. Meningiomas have a peak incidence in the sixth and seventh decades. Most cases are sporadic while but rarely they are familial. Patients who have undergone radiation to the scalp are more at risk for developing meningiomas.
Meningiomas do not arise from the brain substance itself, and therefore are termed "extra-axial" tumors- those tumors which arise within the intracranial or intraspinal space but do not arise from the cells of the brain or spinal cord.
Patients may present with a variety of signs and symptoms related to meningioma. Headache, visual disturbance, seizure,mental status changes and focal neurological deficits are all possible depending on the size and location of the tumor. These tumors are also commonly found "incidentally", or as a consequence of a radiographic investigation (CT, MRI<,angiography) undertaken for other reasons. Meningiomas are readily visualized with contrast CT, MRI with gadolinium, and arteriography.
TREATMENTS
Meningiomas can be "followed" or surgically resected with permanent cure depending on a variety of factors including the size on the tumor, it’s location, how symptomatic the tumor has become and the medical condition of the patient. Stereotaxic radiation is employed in the treatment of meningiomas that are not surgically accessible.
Medulloblastoma
Medulloblastoma is a malignant primary brain tumor that originates in the cerebellum or posterior fossa. Medulloblastoma is one of the family of cranial primitive neuroectodermal tumors (PNET). All PNET tumors of the brain are invasive and rapidly growing tumors that, unlike most brain tumors, spread through the cerebrospinal fluid (CSF) and frequently metastasize to different locations in the brain and spine. These tumors are common amongst children.
TREATMENT
Treatment begins with maximal resection of the tumor. The addition of radiation to the entire neuraxis (brain and spinal canal) and chemotherapy may increase the disease-free survival. This combination may permit a 5 year survival in more than 80% of cases. The presence of desmoplastic features such as connective tissue formation offers a better prognosis. Prognosis is worse if the child is less than 3 years old, there is an inadequate degree of resection, or if there is any CSF, spinal, supratentorial or systemic spread.
Metastasis
A Metastasis is a tumor which occurs in a tissue distant from the origin of the primary cancer. This condition comes about by malignant cells migrating from the primary tumor. Migration can be by the cardiovascular system, the lymphatic system or by the CSF pathways. Many genes need to be activated within malignant cells to allow this process to occur, since normal host tissue cells are made to form sheets of cells, which give rise to the tissues and organs of our body. Recent research has shed light on the abnormal sequencing of genes by these malignant cells which allow them to regain mobility, gain access and egress of blood and lymph vessels, multiply in foreign tissues and draw blood supply by the formation of abnormal blood vessels (angiogenesis) - all functions that normal mature host cells lack. The ability to metastasize is one of the three hallmarks of malignancy.
When a tumor metastasizes, the new tumors are called "secondary" or "metastatic" tumors, and the component cells of these new tumors resemble those of the original tumor. For example, in the event of a lung cancer metastasizing to the brain, the tumors found within the brain are made up of malignant lung tumor cells and not cells from the brain itself. The tumors are therefore referred to as metastatic lung tumors and not primary brain tumors.
Brain metastasis are treated with a variety of modalities depending on the size, number, location and the tissue of origin of the metastasis, the patient’s age and general medical condition as well as overall stage of the primary tumor When metastatic tumors are accessible, surgery remains an excellent treatment option. Multiple metastasis may be addresses at one surgical sitting. Surgery is especially valuable when the cerebral lesion has an unidentified primary tumor; biopsy/removal of the cerebral lesion in this circumstance can provide valuable information (through pathological study) regarding the organ which gave rise to the tumor cells.
Metastatic tumors may also be treated with radiosurgery, chemotherapy, radiation therapy, biological therapy, hormone therapy, laser-immunotherapy, or a combination of these. Ultimately the prognosis of the patient is generally dependent upon the general stage and aggressiveness of the primary tumor and not the presence of metastatic cerebral tumors.
Neurointervential Procedures
Neuro-Endovascular procedures are minimally invasive surgeries of the brain or spine, using vascular access (usually via the arm, leg, or groin) to the affected area. As with other minimally invasive therapies, the trauma to the patient is lessened and the recovery time can be significantly reduced. It is especially useful for patients who are unable, for whatever reason, to undergo a traditional brain or spine operation.
Typically, a catheter is inserted via a small incision, and guided through the arteries to the area of interest. The catheter can then be used to deliver drugs, diagnostic aids such as dyes, coils, embolic materials or restorative equipment such as vascular stents. A wide variety of conditions may be treated by a Neurointerventionalist, including stroke salvage (removal of clots mechanically or by dissolving within cerebral blood vessels), aneurysm rupture, AVM rupture, tumor embolization, and stenting of partially clogged blood vessels.
Normal Pressure Hydrocephalus (NPH)
Normal Pressure Hydrocephalus (NPH)is a chronic type of communicating hydrocephalus whereby the production of spinal fluid becomes equilibrated with the absorption of spinal fluid albeit at a greater volume of CSF within the brain that is normally present. The exact pathophysiologic mechanism of this condition is largly not understood, although indications are that the process involves altered absorption of CSF at the level of the arachnoid granulations, and there is abnormal absorption of CSF fluid from the brain parenchyma via trans-ependymal flow.of CSF. The intracranial pressure may have been elevated early in the course of this disease process, but it does gradually fall, although with a slightly elevated level of pressure. Measurements of CSF pressure are however considered within normal range, since the "normal" range is quite broad. But the pressure for the individual patient would be considered elevated from their pre-disease normal. Because of this gradual equilibration of pressure, patients do not exhibit the classic signs of increased intracranial pressure seen with acute hydrocephalus such as headache, nausea, vomiting, or altered consciousness. Patients instead exhibit a "classic triad" of symptoms which include gait abnormalities (shuffling), urinary incontinence, and dementia. NPH is often confused with Parkinson's disease due to the similarities of gait abnormality. Alzheimer's disease, and senility may also be considered as diagnosis in individuals with advanced NPH due to the progressive mental decline seen with this condition.
NPH may be relieved by surgically implanting a ventriculoperitoneal shunt to drain excess cerebrospinal fluid to the peritoneal cavity within the abdomen where it is absorbed. Once the shunt is in place, most patients have an improvement in their gait and control of urinary incontinence. Success with dementia depends upon the length of time an individual patient has suffered with the symptoms of dementia. Generally those patients who have the best response to shunting are those who have not been affected by dementia for a significant period of time, and dementia was not one of the presenting symptoms of this condition.
Occipital Neuralgia
Occipital neuralgia is a distinct type of headache characterized by piercing, throbbing, or electric-shock-like chronic pain in the upper neck, back of the head, and behind the ears, usually on one side of the head. Typically, the pain of occipital neuralgia begins in the neck and then spreads upwards. Some individuals will also experience pain in the scalp, forehead, and behind the eyes. Their scalp may also be tender to the touch, and their eyes especially sensitive to light. The location of pain is related to the areas supplied by the greater and lesser occipital nerves, which give nerve supply to the scalp of back of the head. The pain is caused by irritation or injury to the nerves, which can be the result of nerve trauma, compression of the nerves by overly tight neck muscles, compression of the nerve as it leaves the spine due to osteoarthritis, or other types of lesions in the neck. In many cases, however, no cause can be found. A positive response (relief from pain) after an anesthetic nerve block will confirm the diagnosis.
Treatment is generally symptomatic and includes physical therapy, cervical traction, anti-inflammatory and muscle relaxant medications, massage and rest. These treatments may be supplemented by local nerve blocks.
In patients who do not improve with conservative management, surgery may be considered. Two procedures are available to help treat this painful condition. Occipital nerve stimulation involved placement of a small electrode overlying the nerve. An electrical current is applied through the electrode which masks the nerve pain. Other patients may undergo resection of this nerve. Both procedures may be very helpful in reducing pain and disability.
Pituitary adenomas
Pituitary adenomas are tumors that occur in the pituitary gland, and account for about 10% of intracranial neoplasms. They often remain undiagnosed, and small pituitary tumors are found in 6 to 24 percent of adults at autopsy.
The diagnosis is generally entertained either on the basis of manifestations of excess hormone secretion; the specifics depend on the type of hormone that is produced by the tumor. These tumors are generally small when discovered as a consequence of the abnormal hormone production and are termed "microadenomas". In other circumstances visual difficulties arising from the compression of the optic nerves by the tumor may bring the patient to medical attention. Generally in these patients, the tumor does not produce any hormones and are much larger at the time of diagnosis. Tumors in this category are termed "macroadenomas". The specific area of the optic nerves compressed by a macroadenoma is the optic chiasm. The peculiar layout of visual fibers in the chiasm leads to a visual deficit termed "bitemporal hemianopsia" which describes the loss of vision in the temporal fields bilaterally.
Pituitary adenomas may be treated with medications that block hormone effects or shut down hormone production by the tumor, or by surgical resection of the tumor. The specific treatment recommended depends on the size of the tumor, the presence or absence of neurological deficits, whether the tumor produces hormone or not, and in the case of a tumor that does produce hormone, whether it responds to medication.
Stroke
Stroke or cerebrovascular accident (CVA) is the rapidly developing loss of brain functions due to a disturbance in the blood vessels supplying blood to the brain. This can be due to ischemia (lack of blood supply) caused by thrombosis or embolism involving a cerebral vessel, or due to a cerebral hemorrhage. Stroke is a medical emergency and can cause permanent neurological damage, medical complications and death if not promptly diagnosed and treated. It is the third leading cause of death and the leading cause of adult disability in the United States and Europe.
Risk factors for stroke include advanced age, hypertension, previous stroke or transient ischaemic attack (TIA), diabetes, high cholesterol, cigarette smoking, atrial fibrillation, migraine with aura, and thrombophilia (a tendency to thrombosis). Blood pressure is the most important modifiable risk factor of stroke.
The traditional definition of stroke, devised by the World Health Organisation in the 1970s, is a "neurological deficit of cerebrovascular cause that persists beyond 24 hours or is interrupted by death within 24 hours". This definition was supposed to reflect the reversibility of tissue damage and was devised for that purpose, with the time frame of 24 hours being chosen arbitrarily. It divides stroke from TIA, which is a related syndrome of stroke symptoms that resolve completely within 24 hours. With the availability of treatments that, when given early, can reduce stroke severity, many now prefer alternative concepts, such as brain attack and acute ischemic cerebrovascular syndrome (modeled after heart attack and acute coronary syndrome respectively), that reflect the urgency of stroke symptoms and the need to act swiftly.
Subrachnoid Hemorrhage
Subarachnoid hemorrhage (SAH) is bleeding into the spinal fluid filled space surrounding the brain, i.e., the area between the two inner meninges called the arachnoid membrane and the pia mater. Subarachnoid hemorrhage may arise due to trauma, tumor, infection, rupture of AVM/aneurysm or as a consequence of hypertensive hemorrhage. Subarachnoid hemorrhage is a medical emergency which can lead to death or severe disability even if recognized and treated in an early stage. Treatment is with neuro-critical care monitoring, medication, control of blood pressure and early neurosurgical investigations and interventions. Subarachnoid hemorrhage results from 5% of all strokes. Approximately 10-15% of patients so afflicted will die before arriving in hospital, and average overall survival is 50%.
The classic symptom of subarachnoid hemorrhage is a sudden severe headache termed a "thunderclap" headache, which most patients describe as ‘"the worst headache of my life". This symptom comprises the only symptom of subarachnoid hemorrhage in about a third of all SAH patients. Other symptoms/signs of SAH may include vomiting, seizures (1 in 14), cranial nerve palsy and stiff neck "meningismus". Confusion, decreased level of consciousness or coma may also occur.be Subconjuctival hemorrhage or subhyaloid hemorrhage (bleeding into eye ) may be visible on gross physical exam or fundoscopy.
As a result of the bleeding, blood pressure often rises rapidly, together with a release of adrenaline and similar hormones. As a result, substantial strain is put on the heart, and cardiac arrhythmias, electrocardiographic changes, myocardial infarction, neurogenic pulmonary edema and cardiac arrest (3%) may occur rapidly after the onset of hemorrhage.
Bleeding into the subarachnoid space may occur as a result of injury or trauma. SAH in a trauma patient is often detected when a patient who has been involved in an accident becomes less responsive or develops neurological signs/symptoms and a CT scan is ordered to evaluate the brain.
Risk factors for subarachnoid hemorrhage are smoking, hypertension (high blood pressure) and excessive alcohol intake; all are associated with a doubled risk for SAH. Some protection of uncertain significance is conferred by Caucasian ethnicity, hormone replacement therapy, a higher than normal cholesterol and the presence of diabetes mellitus.
Acute Subdural Hematoma (SDH)
An acute subdural hematoma (SDH) is a form of traumatic brain injury in which blood gathers between the dura (the outer protective covering of the brain) and the arachnoid (the middle layer of the meninges). This bleeding often leaks into the subarachnoid space as well. Unlike the epidural hematoma which is caused by a disruption of the meningeal arteries located on the external surface of the dura mater, an acute subdural hematoma is most often caused by motor vehicle accidents and falls, during which the brain within the skull is exposed to rapidly changing velocities which severely distort the brain and may stretch and tear the brain itself leading to disruption of small arterioloes with resultant hemorrhage and swelling of the brain. This type of brain injury is termed a "shear injury" and is the result of rotational forces being applied to the brain. The high mortality rate associated with SDH is primarily related to the brain damage as a result of this shear injury to the brain.
Subdural hemorrhages are often associated with an increase in intracranial pressure (ICP), which can cause compression the surrounding brain tissue and interference with delivery of blood supply to the brain leading to stroke. More often than not, the increased ICP is a result of brain swelling from damage to the brain parenchyma and less so from the mass of the SDH. Acute subdural hematoma therefore has a high mortality rate and is a severe medical emergency which requires specialized care in a neurological intensive care unit.
Chronic Subdural Hematoma (SDH)
Chronic subdural hematoma (SDH) is a collection of blood which collects between the dura mater and the underlying arachnoid. Unlike an acute subdural hematoma, this type of hematoma is the result of venous bleeding, usually caused by tearing of the "bridging" veins of the brain. These bridging veins course between the dura and the brain itself. Due to brain atrophy which leads to our brains shrinking in size as we age, the subarachnoid space increases in size, putting these bridging veins under stress. Low energy head trauma therefore can stretch and rupture these bridging veins leading to a chronic subdural hematoma. Brain disruption is uncommon, as is brain swelling. Symptoms related to a chronic subdural hematoma are largely related to the area of the brain compressed by the hematoma. Often the initial symptoms may be very subtle. This condition is commonly seen in the elderly and in alcoholics, who usually have evidence of significant brain atrophy. This condition is also more common in patients on anticoagulants, such as coumadin and aspirin. Patients on these medications can develop subdural hematoma with only minor injury.
It is important that a patient receive medical assessment, including a complete neurological examination, after any head trauma. A CT scan or MRI scan will usually detect significant subdural hematomas.
Treatment of a subdural hematoma depends on its size and rate of growth. Small subdural hematomas can be managed conservatively, with medical surveillance during a reasonable amount of time over which the body may resorb the intracranial blood. Large or symptomatic hematomas require surgery. This can often be accomplished by a Burr-hole craniotomy, during which a surgeon creates one or two small holes in the skull, opens the dura mater and allows the chronic subdural to drain.
Trigeminal neuralgia (Tic douloureux)
Trigeminal neuralgia is the most common of the neuralgia syndromes.
An estimated 1 in 15,000 people suffers from trigeminal neuralgia, although numbers may be significantly higher due to frequent misdiagnosis. It usually develops after the age of 40, although there have been cases with patients being as young as three years of age.
The pain associated with trigeminal neuralgia is intermittent and feels like bursts of sharp, stabbing, electric-shocks. This pain can last from a few seconds to a few minutes.
This intense pain involves the eyes, lips, nose, scalp, forehead, and/or jaw. Trigeminal neuralgia is considered by many to be among the most painful of conditions.
To describe the pain sensation, patients describe a trigger area on the face, so sensitive that touching or even air currents can trigger an episode of pain.
The intermittent sharp pain associated with trigeminal neuralgia interferes with common daily activities such as eating, speaking, laughing and sleep. They live in fear of unpredictable painful attacks, which leads to sleep deprivation and under-eating. The condition can lead to irritability, severe anticipatory anxiety and depression, and life-threatening malnutrition. Suicidal depression is not uncommon.
Some patients will have a muscle spasm which led to the original term for TN of "tic douloureux" ("tic", meaning 'spasm', and "douloureux", meaning 'painful', in French).
There are several different causes of trigeminal neuralgia and because people’s symptoms vary, many cases may go un-diagnosed or are difficult to diagnose. Some of the factors that contribute to trigeminal neuralgia are:
- Nerve damage or trauma relating to a dental procedure, surgery, or accident.
- A vessel that is pressing directly on the root of the nerve.
- A tumor pressing on the nerve. (rare)
- Advanced MS that can cause the Myelin Sheath that covers the nerve to deteriorate. (rare)
- Lyme Disease trigeminal neuralgia.
- Post-Herpetic (shingles) trigeminal neuralgia.Other viral infections.
- Trigeminal Neuralgia Diagnosis
MRI can be used to determine whether a tumor or multiple sclerosis is causing the pain of trigeminal neralgia. Otherwise, no test can determine with certainty the presence of trigeminal neuralgia. Tests can, however, help rule out other causes of facial disorders. Trigeminal neuralgia usually is diagnosed based on the patient's description of the symptoms.
Trigeminal Neuralgia Treatment
Medications may be used as a first line treatment for trigeminal neuralgia and are usually anti-seizure medicines. These include in particular "tegretol", "trileptal", neurontin" and "lyrica." If medication is not helping or patients are experiencing side effects from the medication, then a procedure can be considered.
The surgical treatment of trigeminal neuralgia includes several surgical procedures including microvascular decompression, radiofrequency rhizotomy, glycerol rhizotomy, balloon rhizotomy, and stereotactic radiosurgery).
Surgery may be recommended, either to relieve the pressure on the nerve or to selectively damage it in such a way as to disrupt pain signals from getting through to the brain. In trained hands, surgical success rates have been reported at better than 90 percent.
Of the five surgical options, the microvascular decompression (MVD) is the only one which preserves the trigeminal nerve and addresses the nerve compression by cerebral blood vessels when they are the cause of trigeminal neuralgia. In this procedure, the surgeon enters the skull through a small opening behind the ear. The nerve is then explored for an offending blood vessel, and when one is found, the vessel and nerve are separated or "decompressed" with a small pad. When successful, MVD procedures can give permanent pain relief with little to no facial numbness.
Nerve-Injuring" techniques can also be very effective in treating trigeminal neuralgia. These methods of nerve injury include "percutaneous" procedures performed through a needle, and radiosurgical procedures accomplished by use of computer-focused radiation beams.
Percutaneous trigeminal nerve injuring procedures, also known as "rhizotomies," use needles or catheters that enter through the face into the opening where the nerve first splits into its three divisions. Excellent success rates using these "percutaneous" surgical procedures have been reported.These techniques include "radiofrequency", glycerol" and "balloon" methods. In a radiofrequency rhizotomy, a surgeon uses an electrode to heat the selected division or divisions of the nerve. Done well, this procedure can target the exact regions of the errant pain triggers and disable them. This technique is particularly useful for patients with pain in the cheek or jaw, or the lower portions of the face. Glycerol rhizotomy involves injecting glycerol, an alcohol like substance, into the cavern that bathes the nerve. This liquid can injure the nerve just enough to disrupt the pain signals. Balloon compression involves compressing the nerve against the skull, again, just enough to stop the passage of pain signals. The balloon technique is particularly useful for patients with ophthalmic division pain, that is, pain in the forehead or eye.
Another procedure for treating trigeminal is stereotactic radiosurgery. In this technique, super-focused radiation beams are aimed at the nerve, to disrupt the pain signals. This procedure is a one day, minimally invasive, out-patient procedure, that does not require anesthesia. The procedure is done with only the most advances stereotactic radiosurgery devices such as the Gamma Knife, or specialized linear accelerators such as the Cyberknife. No incisions are involved in this procedure. Radiation is used to bombard the nerve root, targeting the same point where vessel compression is normally found. This procedure is particularly favorable for patients who are older, have serious medical problems, or who have to stay on blood thinners.
These nerve injuring procedures are useful for patients who are elderly, have significant medical problems, have failed MVD, or have multiple sclerosis (in whom blood vessel compression is not felt to be the cause of the trigeminal neuralgia). The nerve-injuring techniques are minimally invasive, out-patient procedures. The main disadvantages to these techniques include the risk of producing numbness or dysethesias (abnormal feelings) in the face as well as a higher chance of recurrence with time (because the nerve can regrow.)